For nearly a decade, Judy Pidgeon packed away her wanderlust—and indeed, much of her life—to look after her mom, who was profoundly disabled by a stroke. Recalling her mother’s fierce desire not to end up in institutional care, Pidgeon returned with her husband to the family home in Calgary, trading international travel and wilderness work for enemas, catheters, mechanical lifts and constant vigilance. That caregiving journey ended in December 2012, when Sophie May Oss died at age 89. It cost Pidgeon prime years of her career, not to mention emotional energy and income. What’s more, home care, the publicly funded system set up expressly to keep life on an even keel in situations exactly like this, seemed intent on charting its own predetermined course rather than paying heed to the needs of Pidgeon’s mother—let alone to the needs of the family member whose presence was keeping yet another senior from plunging into more expensive forms of care. Says Pidgeon, a wiry 61-year-old whose close-cropped hair hints of a do-it-my-way approach to life, “Dealing with the home care system was the single most stressful part of those 10 years.”
In theory, Alberta’s home care system makes good sense. Individuals who need support are assessed by an Alberta Health Services (AHS) case manager, who develops a plan allotting time for such services as bathing, dressing, toileting, giving medication, ventilator upkeep and palliative care. The work is contracted out to providers, who hire frontline workers (health care aides, in provincial parlance) to deliver the care under the supervision of nurses—with support from occupational therapists, nutritionists and other specialists as needed.
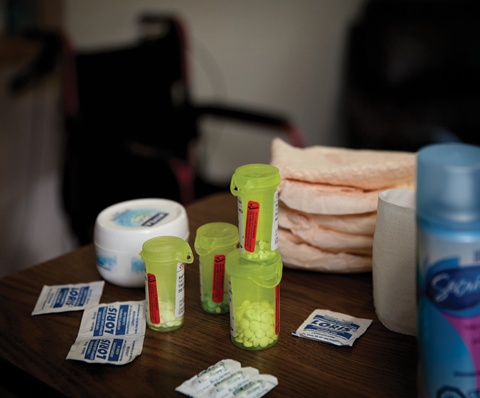
In practice, the system is being chipped away at the very time when an expanding number of seniors need care. Housekeeping help, which Pidgeon’s mom had received in earlier years while recovering from a back injury, was not included in her care plan after the stroke. The time allotted in her care plan shrank from 26 hours a week to as little as eight, even as her needs escalated. The care also shifted from non-profit to for-profit providers, including the Toronto-based CBI Health, which took over all contracts in Oss’s area of Calgary during a regional move to zone-based care. A revolving parade of health care aides began coming to the door, many lacking training in key tasks—and each unfamiliar with Oss and her needs. With minimal pay and no benefits, some aides worked multiple jobs to make ends meet, and arrived at Oss’s house late or overtired and distracted, resulting in accidents. Pidgeon’s calls to the agency led to long periods on hold while listening to advertisements for fee-based services, only to have concerns dismissed as isolated rather than systemic issues. “It was a profit-first, care-second business model,” Pidgeon says.
Desperate for relief, Pidgeon occasionally booked a bed for her mom in a nearby nursing home under a caregiver respite program that has also lost funding over the years. But her mom returned depressed and diminished. Clearly, home was best, but Pidgeon was bearing the brunt. “By last year, I thought I might die before mom of a stroke or heart attack,” she says. “And you know what? It seemed like a good idea.”
Pidgeon’s story is far from unique. Every sixth senior receives home care, according to the Canadian Home Care Association; 98 per cent have an informal, unpaid caregiver, most often a family member. Across Canada, five million family caregivers provide as much as 75 per cent of their loved ones’ care, a service worth $25-billion a year. But many (especially those looking after high-needs seniors) are at a breaking point, says a 2012 Health Council of Canada report tellingly titled Seniors in Need, Caregivers in Distress.
Family caregivers and the home care workers who support them are foundational to our entire healthcare system. Together, they enable people to live longer in their own homes (where most want to be) at less than half the cost of nursing-home care and a twentieth the cost of being in hospital, according to Dr. Samir Sinha, who leads Ontario’s Seniors Strategy. Yet Alberta caregivers and care workers alike relate tales of shrinking care plans, disrupted relationships and a disjointed system that discourages input even though complaint seems the only way to effect change. “If the government continues to download eldercare to families without providing suitable support, the system will fail,” Pidgeon predicts. “Hospitals will end up with many more beds filled with elderly disabled, plus families will be thrust into crisis situations they have no way of handling.”
The Alberta government’s own Continuing Care Strategy, in effect since 2008, calls for “enhanced and expanded home-support services,” including increased daily care hours and more respite for informal caregivers. Its guiding health document, Vision 2020, “puts patients at the centre” and commits to “providing the right service, in the right place, and at the right time.” But actions speak louder than words. With the number of nursing home (or long-term care) beds stalled at 14,554 (despite Conservative election promises to add 1,000 beds), a recent Health Quality Council of Alberta (HQCA) study found 7 per cent of hospital beds were being taken up by seniors waiting for appropriate places to live. “The government promised all sorts of things so you don’t have to move into a long-term care facility,” says Sandra Lyons, executive director of the University of Alberta’s Institute for Continuing Care Education and Research, who also coordinates care for her mother. “So they stopped building long-term care facilities, but they didn’t put the money into the community supports that are necessary in order to age in place.”
To be fair, Alberta’s home care budget has been inching upward. Last year’s $496-million budget is up 9.5 per cent from the previous year, and expenditures were $507-million according to the AHS annual report. But the home care client list is expanding apace, from 97,326 in 2011, when the first baby boomers crossed the 65-year line, to 108,855. What’s more, Alberta trails other provinces in its percentage of health dollars invested in home care, at just 2.4 per cent compared to 4.1 per cent across Canada and 6.4 per cent in New Brunswick. By 2031, when the last baby boomers turn 65, Alberta will be home to 923,000 seniors, twice as many as today. Unless the budget trajectory shifts, need will far outstrip home care capacity.
Alberta stopped building nursing homes, but hasn’t put enough resources into the home care system.
The care needed by the typical client is rising as the senior population ages—and as acute care patients are discharged earlier from hospital. Pilot projects in Alberta and elsewhere have seen those clients doing well at home, but only with consistent and adequate support. All too often they’re left waiting for essential therapy, equipment and care, says Sandra Azocar, who hears many such stories as executive director of Friends of Medicare. “If people cannot go home because they can’t receive the service they require, core issues such as wait times are not going to be addressed.”
Publicly funded home care has also become increasingly focused on core medical needs, despite growing evidence that housecleaning, transportation, companionship, caregiver respite and other “soft services” are crucial to keeping seniors at home. Those services may be available in the marketplace, but at a cost many seniors cannot afford, says Elaine Roberts, who led house meetings about seniors’ needs for the Greater Edmonton Alliance. “Seniors are saying we’re not looking for a handout, but there has to be more attention to ability to pay.”
Liberal health critic Dr. David Swann echoes that view. He and his wife needed extra help while looking after his mother in their home for six years, even though both are medical doctors. “We were able to pay for a caregiver to come in, but many are not, and that’s where the rubber hits the road,” he says. “Families are financially and emotionally and physically exhausted because they’re trying to fill that gap. Are we a society that’s going to ensure that we care for our most vulnerable elderly, who created this province? Or are we simply going to abandon them to chance—and to private, for-profit providers?”
Critics say Alberta Health Services is doing exactly that. In a surprise move that threw thousands of home care providers and clients into panic, this summer AHS contracted the lion’s share of home care in its Edmonton and Calgary zones to a handful of large private corporations, some headquartered in Ontario, displacing dozens of smaller providers with local roots. Bidders were sworn to secrecy throughout the process, which happened without consultation and was fundamentally flawed, says Bruce West, who spent decades behind related government desks before becoming executive director of the Alberta Continuing Care Association. “The government went to the team that contracts for hospital beds and linen services and used that same procurement mentality as if these were widgets rather than direct care to people in communities.”
Edmonton was particularly hard hit by a shift to zone-based delivery—the same shift that occurred in Calgary while Pidgeon was looking after her mom. That shift gave each winning agency a monopoly in its area, raising questions about the province’s stated commitment to patient choice. What’s more, some of the providers shunted aside have an admirable record of embedding home care within a larger package of holistic support. Those include Strathcona County and the City of Leduc, which used local funds to subsidize services such as housekeeping and caregiver respite—and to pay home care workers significantly more than the provincial dollars allocated. “AHS has said its direction is more community-based,” West says. “Yet here we have municipal entities removed from providing care to their own citizens.”
In response to concerted outcry, three Edmonton co-ops providing home care to their own disabled residents got their contracts back. “We should have paid more attention to the needs of some individual Albertans,” AHS president Chris Eagle said in announcing the reversal. As NDP health critic David Eggen puts it, “The Eagle was forced to eat some crow.” Still besieged by protests, Health Minister Fred Horne instructed newly appointed health administrator Janet Davidson to review the contract process. In mid-July, 10 “congregate living providers” and three others with “unique population needs” were invited to renew their contracts. Examples include Lifestyle Options, a retirement community whose around-the-clock staff provides a mix of home care and more intensive care under contract with AHS, and Edmonton’s Operation Friendship, whose inner city lodges serve seniors with addictions and mental-health concerns.
Throughout the summer, thousands of other clients were “transitioned” to new providers, often losing trusted care aides. From day one, clients were calling with horror stories, says Sue Dittrich, who has provided care for 14 years with Strathcona County Family Services. The calls echoed Pidgeon’s experience: Missed appointments. Untrained workers. Rushed care. Errors. “When everybody works together, people can get a tremendous amount of help,” says Dittrich. “But when a link breaks, that’s when people fall through the cracks.”
The consolidated home care contracts continue a shift that puts the majority of Alberta’s home care delivery into a few corporate hands. AHS predicts the move will save $18-million. The NDP’s Eggen stands among those who say any savings will come on the backs of frontline workers and the families they serve. “The public health system was set up because we knew that if we looked after each other in the most equitable way possible and pooled money to do that, no one would get left behind,” he says. “I see this latest chapter as nothing less than breaking that sacred trust.” By contrast, West, whose association includes for-profit providers, calls concern about corporate ownership a “red herring that allows us to ignore the fact that none of these organizations are adequately funded in relation to what is expected.” Exceptional private providers do exist, but studies by both the HQCA and the Parkland Institute indicate that, on average, care tends to be inferior in for-profit settings, largely due to fewer and less-qualified staff.
Contract details have not been made public, another reason to avoid using private suppliers for a fundamental public good. But there will be less government money. In the past year, the government cut the time allotted for workers to do typical tasks, and stopped paying travel time. Mileage payments, previously eliminated in cities, are now gone in rural zones. At a town hall meeting that attracted dozens of incensed home care workers, Sharon Smythe said she’s been earning $15 an hour and driving 60,000 km a year to serve clients south of Edmonton for We Care, one of Alberta’s largest private contractors. “Mileage is more than my paycheque,” she said. “Without it, it doesn’t pay to leave home.” The loss of mileage, coupled with reduced wages, is expected to heighten a chronic shortage of care workers in rural Alberta, forcing seniors and other vulnerable people to uproot.
Home care RNs and LPNs across the province are losing their jobs under a new AHS staffing model that puts more frontline work in the hands of health care aides. We Care worker Shannon Comeau believes it’s a calculated move: “We’re going to be the backbone of healthcare in a very short time, and they want to be sure they’re not paying the backbone very much.” West predicts that unintended consequences will include a shortage of workers and a push to unionize. “I can’t help but think AHS painted a very big ‘X’ on the backs of those that got contracts. Not only are salaries dropping, but there are now just a few agencies that need to be organized.”
Unlike RNs and LPNs, health care aides are not regulated, and their training consists of a six-month certificate program that not all employers require. “We put tiny toddlers into daycare and playschools with people who aren’t well educated for the job and pay them shitty wages, and then at the end of life we have these seniors who have worked their whole lives and raised their own families and we do the very same thing,” says a frontline worker with a for-profit firm who asked not to be identified. “Really and truly, we need to be better educated and regulated—and we need to be treated fairly. We’re dealing with vulnerable people in the late stages of life who deserve respect. We’ve got to do our absolute best to give them that.”
At the core, the government’s reluctance to meet escalating home care need reflects a silo mentality that fails to connect the budgetary dots between service cutbacks and costs elsewhere in the system, says Irene Martin, executive director of Alberta Senior Citizen Housing. Working with ill family and friends, she has seen how the miserly doling out of things as basic as beds, diapers and time results in bedsores, hospitalization and diminished humanity. Such environments make clients, staff and families angry, she adds, and that’s not good for anybody’s health, let alone healthcare budgets. “If we don’t integrate all these chopped-up little pieces, we’re never going to make it.”
Tina MacDonald discovered the value of integration while caring for her husband, Duncan, during his final five years of life. As health consultants, the MacDonalds knew how the system works—and who to call when it doesn’t. Yet they too bounced from silo to silo until Duncan was diagnosed with a neurological disorder and began attending Edmonton’s interdisciplinary ALS clinic. The entire team, home care included, met with the family, providing a place to troubleshoot challenges as Duncan’s mobility rapidly declined. “It gave home care a framework to fit within, and we didn’t have such a problem with things falling off the edges,” reflects Tina, who cared for Duncan along with her son, some home care support and a dizzying array of privately paid specialists.
Among international models of integrated home care, Denmark surfaces often. In stark contrast to Canada, Denmark invests equally in home and institutional care; as a result, it has closed thousands of hospital beds in recent decades without expanding long-term care. Citizens over 75 receive regular home visits that pay attention to such proactive measures as diet, exercise, fall prevention and social networks as well as home upkeep and caregiver needs. It’s an approach that matches Swann’s prescription for home care: “Moving upstream is what’s needed,” he says, “right to primary prevention.”
Today’s technology offers the potential to connect and inform teams in ways that weren’t possible in the past, Swann adds. Indeed, the Health Council of Canada calls technology the “missing link” that could integrate health care, for example by making electronic health records available at home and enabling doctors to make virtual house calls.
Compensating caregivers means investing money, as does paying aides a living wage and focusing on preventive health care.
I meet some family caregivers who have a self-managed care program under which AHS allots families money to hire and pay workers themselves rather than depending on outside providers. Anna Burrowes and her father, for example, have hired a live-in caregiver to look after her mom, who at age 62 is as dependent as a newborn due to a rare degenerative disease. While more complex than many families can manage (“It’s like owning your own business,” Burrowes says), this approach shows what can happen when family is at the centre rather than on the periphery of the team.
As the women describe their caregiving with frank, black humour, it’s clear they are devoting huge chunks of their lives to the task. Were they living in Australia, the UK or Sweden, they could expect to be paid for their time. Not here. Short-term employment insurance is available to citizens looking after dying family members, and Alberta recently joined other provinces in ensuring that employees can return to their previous jobs after eight weeks of caregiving. But Albertans without employment receive no financial support.
Judy Pidgeon (who petitioned for compensation while looking after her mom, but was repeatedly refused) advocates extending self-managed payment to full-time family caregivers who prove they are dependable, responsible and honest. Government’s reluctance to do so reflects a philosophy that families should look after their own, West notes. “But that’s a holdover from the old nuclear family concept and doesn’t match today’s reality.”
Of course, compensating family caregivers means investing more government money, as does paying healthcare aides a living wage, turning silos into teams and focusing more on preventive health care. The recent reinstatement of contracts to Edmonton providers demonstrates that public outcry can shift the political course. But fundamentally restoring home care will take sustained persistence. Politicians respond to light (accurate information) and heat (public confrontation), Swann says. “Generally we’re good at turning on the light in this society—not so good at turning up the heat.”
Cheryl Mahaffy is a journalist and long-time contributor to Alberta Views.

